Contents
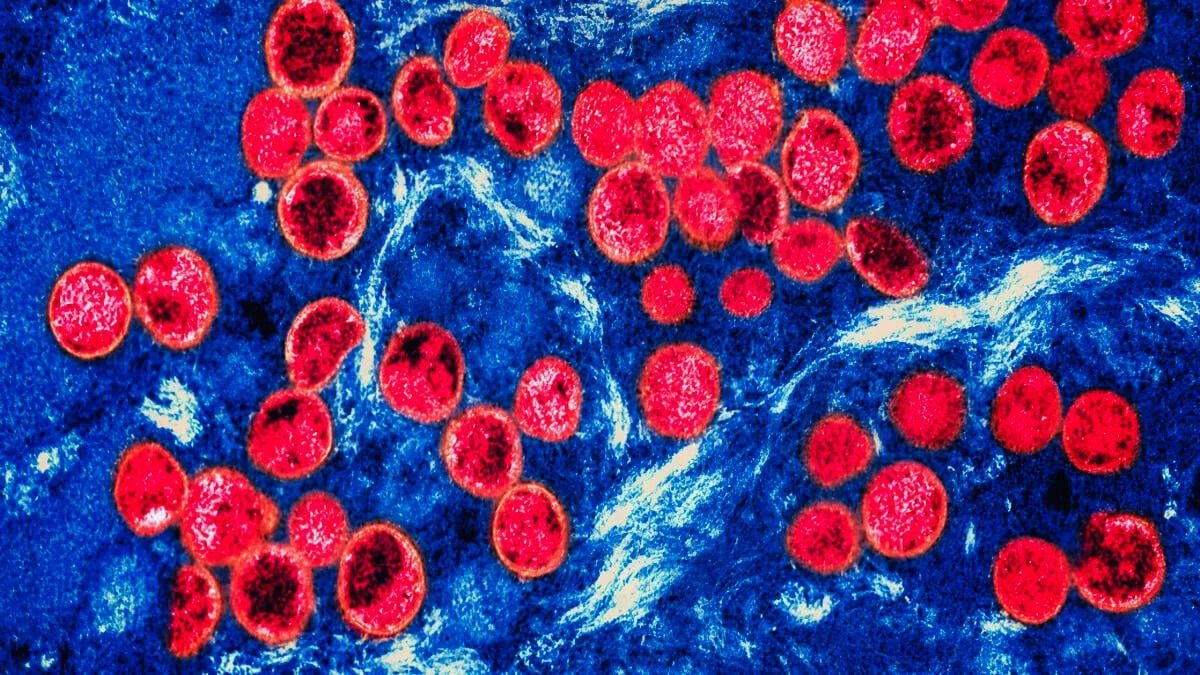
Introduction to Mpox and Recent Outbreak, Mpox outbreak
Mpox, also known as monkeypox, is a zoonotic viral disease caused by the monkeypox virus, belonging to the Orthopoxvirus genus. This virus shares a close resemblance to the variola virus, responsible for smallpox, although it generally results in a milder illness. Historically, mpox has been confined largely to Central and West Africa, where it circulates among various animal reservoirs, particularly rodents and primates. The disease was first identified in humans in 1970 in the Democratic Republic of Congo. Since then, sporadic outbreaks in humans have been documented, usually linked to direct contact with infected animals or through consumption of bushmeat.
The recent outbreak of mpox has drawn significant attention due to its unprecedented spread beyond the African continent, prompting the World Health Organization (WHO) to designate it a global health emergency. This marks a significant escalation, reflecting the rapid increase in confirmed cases and the geographical dispersion of the virus. By mid-2023, confirmed mpox cases have been reported in over 50 countries across five continents, representing a dramatic shift from its historical endemic regions. This global spread has raised alarms about potential widespread transmission, underpinning the urgency of a coordinated international response.
As of the latest updates, the reported global case count stands in the tens of thousands, with notable clusters identified in Europe, the Americas, and Asia. Initial responses from health authorities have varied, ranging from aggressive contact tracing and quarantine measures to public health advisories and vaccine rollouts. The swift declaration of a global health emergency by the WHO aims to mobilize international cooperation, enhance surveillance, and support countries in implementing effective containment strategies. Understanding the dynamics of this outbreak and the disease’s epidemiology is crucial for developing robust public health interventions to mitigate its impact.
Criteria and Process for Declaring a Global Health Emergency, monkeypox global health emergency
When confronted with potential global health threats like the mpox outbreak, the World Health Organization (WHO) follows a rigorous framework to declare a Public Health Emergency of International Concern (PHEIC). This framework is pivotal for galvanizing international coordination and response for health crises. The decision is driven by a defined set of criteria, which include assessing the impact on public health, the capability for the disease to spread internationally, and the necessity for a harmonized global response.
The deliberation process for declaring a PHEIC is meticulous. Initially, the WHO closely monitors the situation to collect comprehensive data. This data collection involves surveillance systems and information from affected countries. Subsequently, an Emergency Committee comprising international health experts is convened. These experts provide independent advice based on the outbreak’s epidemiological data, potential societal disruption, and existing containment measures.
Once assembled, the Emergency Committee engages in a thorough review, considering factors such as the outbreak’s severity, rate of transmission, and whether it exceeds a nation’s response capacity. The Committee’s recommendations are crucial as they inform the WHO’s Director-General, who holds the ultimate authority to declare a PHEIC.
Consultations and input from global health experts also play a significant role. This inclusive approach ensures a holistic understanding of the threat and aids in determining the appropriate level of response. During their consultations, the Committee may also consider the effectiveness of implemented countermeasures within the affected regions.
Examining historical PHEIC declarations provides insight into how these emergencies are managed. For instance, the Zika virus outbreak in 2016 and the Ebola crises in 2014 and 2019 spotlight the intense global collaboration required. Each of these declarations necessitated swift, coordinated international responses to monitor, manage, and mitigate the outbreaks.
The comprehensive framework and rigorous process supporting the declaration of a PHEIC underscore the WHO’s commitment to safeguarding global health. By meticulously evaluating the impact, transmission potential, and need for an international response, the WHO ensures that such declarations prompt timely, effective, and cohesive global health strategies.
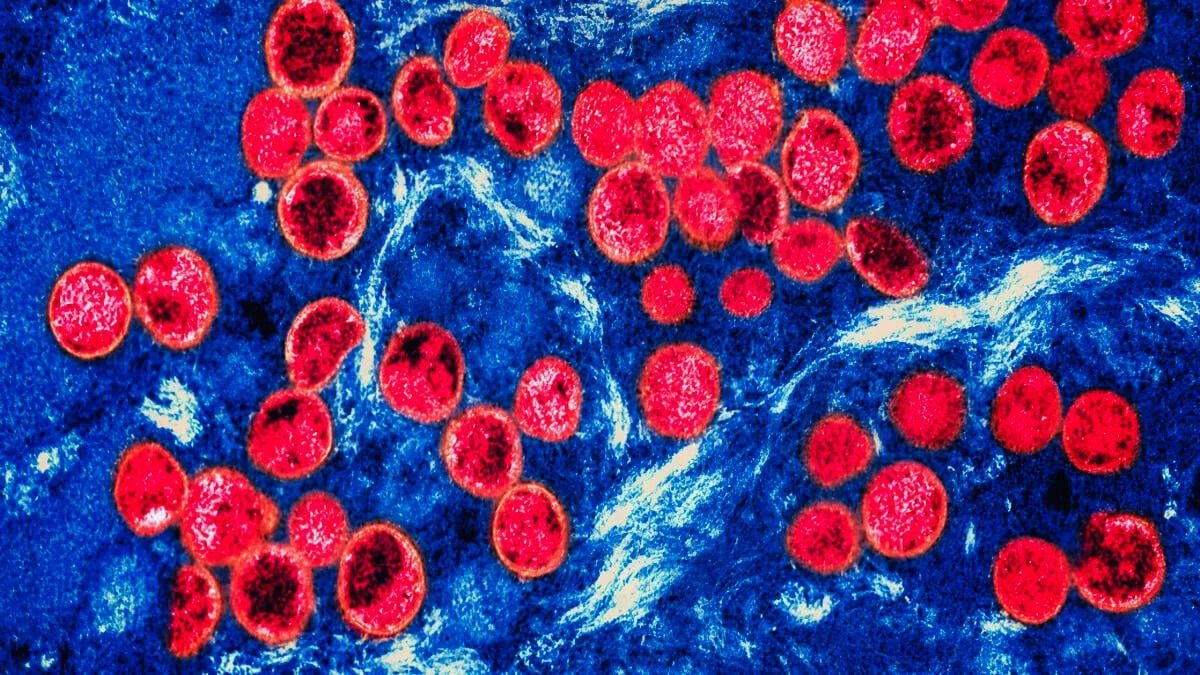
Implications of a Global Health Emergency Declaration, Mpox transmission
The World Health Organization’s declaration of the Mpox outbreak as a global health emergency has profound implications for a myriad of stakeholders. For governments, this declaration translates to an urgent need for heightened surveillance and faster diagnostic capabilities. Nations are now compelled to enhance their public health infrastructures, ensuring timely and accurate reporting of Mpox cases. Furthermore, the international travel sector may experience renewed scrutiny as governments consider potential travel restrictions to prevent further spread.
Healthcare systems are also at the forefront of this response. The declaration necessitates a potential reallocation of resources, emphasizing the importance of efficient vaccine deployment and robust public information campaigns. Hospitals and clinics will need to prioritize Mpox vaccination efforts while simultaneously managing other essential healthcare services. In addition, healthcare professionals will be tasked with educating the public on preventive measures, ensuring that communities understand and adhere to guidelines aimed at curbing the outbreak.
The general public’s response is equally critical in this scenario. Individuals are expected to adopt preventive measures such as frequent handwashing, wearing masks, and avoiding close contact in high-risk areas. Behavioral changes, driven by increased awareness and governmental advisories, could significantly impact the trajectory of the outbreak. Public adherence to health guidelines will be instrumental in mitigating the spread of Mpox.
Beyond immediate measures, the declaration will undoubtedly influence global health policies and funding. The international community is likely to see a boost in funding allocated for Mpox research, vaccine development, and public health initiatives. Additionally, this situation underscores the importance of international collaborations in addressing health crises. By fostering cooperation among nations, the global health emergency declaration paves the way for a coordinated effort in combating Mpox and preventing future outbreaks.
Steps Forward and Future Preventive Measures, public health response to Mpox
As the global community grapples with the mpox outbreak, it is imperative to implement robust strategies to curtail the virus’s spread. One of the primary steps forward is enhancing contact tracing. By identifying and isolating individuals who have come into contact with infected persons, health authorities can significantly reduce transmission rates. Advanced contact tracing mechanisms, combined with digital tools, can streamline the process, ensuring prompt and efficient identification of potential cases.
Vaccination campaigns play a pivotal role in preventive measures against mpox. Broadening the coverage and accessibility of vaccines, particularly in high-risk regions, is crucial. Public health agencies must invest in widespread immunization drives, utilizing both existing vaccines and those under development. Outreach initiatives are necessary to educate communities on the benefits of vaccination, thereby increasing public trust and participation.
Strengthening healthcare infrastructure, particularly in vulnerable regions, is another critical component. Bolstering healthcare facilities, ensuring an adequate supply of medical equipment, and training healthcare personnel to handle mpox cases can enhance readiness and response capabilities. Additionally, international aid and support should be directed towards areas with limited resources to build a robust frontline defense against the virus.
Research and development efforts are indispensable in the fight against mpox. Continuous scientific investigation into the virus’s behavior, transmission, and potential treatments can pave the way for innovative solutions. Collaborative endeavors between research institutions, pharmaceutical companies, and governments can accelerate the development of effective antivirals and other therapeutic measures. Furthermore, improving outbreak response mechanisms through data analytics and predictive modeling can optimize intervention strategies and minimize future risks.
Global cooperation remains a cornerstone in the endeavor to prevent future outbreaks. International organizations such as the World Health Organization (WHO) play an instrumental role in coordinating efforts, sharing information, and providing guidelines. By fostering an environment of global solidarity and resilience, the world can better prepare for and mitigate the impacts of infectious disease outbreaks. Establishing a unified global response framework, underpinned by readiness and mutual support, is essential in safeguarding public health and ensuring long-term stability.
OUR SITE: toinewsalert.com





