Contents
Introduction to the Fungal Infection
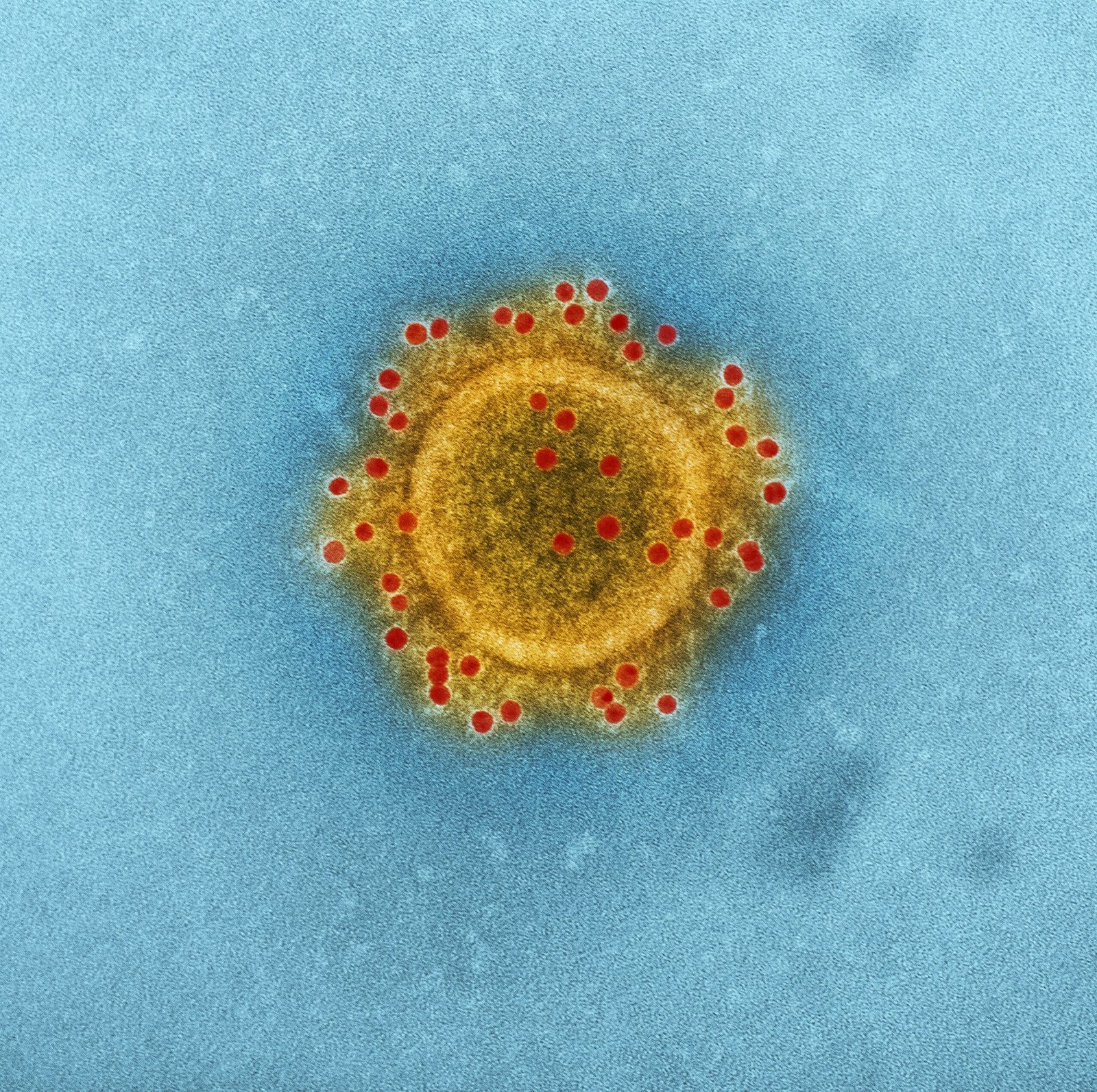
The recent identification of the first U.S. case of a sexually transmitted fungal infection in New York City marks a significant development in public health. The infection, caused by the fungus Aspergillus fumigatus, differentiates itself from more common fungal infections due to its mode of transmission and potential implications for public health. Unlike typical fungal infections that are generally transmitted through environmental exposure or direct contact, this particular strain represents a novel pathway of infection.
Aspergillus fumigatus is a pathogenic fungus known primarily for causing respiratory illnesses, especially in immunocompromised individuals. Its ability to adapt and survive in various environments makes it a formidable pathogen. This newly discovered mode of transmission via sexual contact underscores the adaptive nature of fungal pathogens and raises concerns about potential outbreaks and the need for revised public health strategies.
The detection of this case in New York City is noteworthy for several reasons. Firstly, it highlights the city’s role as a major global hub where diverse populations and high-density living conditions may facilitate the spread of novel infections. Secondly, it underscores the importance of vigilant public health surveillance and research in identifying emerging infectious diseases. The identification of this sexually transmitted fungal infection necessitates a reevaluation of current diagnostic and treatment protocols, as well as public awareness campaigns to educate the population on preventive measures.
Understanding the characteristics of this fungal infection and its implications sets the stage for a deeper exploration into its impact on public health. This discovery not only challenges existing paradigms but also emphasizes the need for continuous monitoring and innovation in the field of infectious disease control. The subsequent sections will delve into the specifics of the case, its clinical manifestations, and the broader public health response.
Case Details and Diagnosis
The first documented U.S. case of a sexually transmitted fungal infection was identified in New York City, marking a significant development in the field of infectious diseases. The patient presented with symptoms that were initially nonspecific, including persistent itching, discomfort in the genital area, and unusual discharge. These symptoms prompted the individual to seek medical attention, leading to a thorough examination by healthcare professionals at a local clinic.

Upon initial consultation, the medical team conducted a series of diagnostic procedures to pinpoint the cause of the symptoms. Standard tests for common sexually transmitted infections (STIs) such as gonorrhea, chlamydia, and trichomoniasis returned negative. Given the persistence of the patient’s symptoms, the healthcare providers expanded their diagnostic scope to include less common pathogens. A comprehensive swab of the affected area was taken and sent to a specialized laboratory for fungal culture and polymerase chain reaction (PCR) testing.
The timeline of events unfolded over several weeks, during which the patient’s condition remained stable but unresolved. The laboratory results eventually revealed the presence of a previously undocumented fungal species capable of sexual transmission. This discovery was pivotal, as it highlighted the potential for fungi to be transmitted in ways not traditionally recognized. The medical team, comprising infectious disease specialists and mycologists, promptly reported the case to public health authorities and initiated an investigation to understand the origin and transmission dynamics of the infection.
Initial treatment steps included antifungal medication tailored to the specific fungal species identified. The patient was closely monitored, and follow-up visits were scheduled to assess the effectiveness of the treatment regimen. This case underscores the importance of considering a broad differential diagnosis in patients with persistent genital symptoms and the need for ongoing research into emerging infectious agents.
Transmission and Spread
The first U.S. case of a sexually transmitted fungal infection, identified in New York City, marks a significant development in the understanding of fungal diseases. Unlike more commonly known modes of fungal transmission, such as through inhalation of spores or direct contact with contaminated surfaces, this particular fungal infection is transmitted through sexual contact. This mode of transmission presents unique challenges in terms of controlling and preventing its spread.
Sexually transmitted fungal infections differ from other fungal infections in several key aspects. Traditional fungal infections, such as athlete’s foot or ringworm, are typically spread through skin-to-skin contact or contact with contaminated objects. In contrast, the sexual transmission route involves the direct exchange of bodily fluids, which can facilitate the spread of the pathogen in intimate settings. This highlights the importance of sexual health education and preventive measures in curbing the transmission of this new fungal infection.
Risk factors for contracting this sexually transmitted fungal infection include having multiple sexual partners, unprotected sex, and a compromised immune system. Populations most at risk include young adults, individuals with underlying health conditions, and those who engage in high-risk sexual behaviors. Understanding these risk factors is crucial for healthcare professionals to identify and target vulnerable groups for education and intervention.
Experts emphasize the importance of awareness and prevention measures to mitigate the potential spread of this infection. Dr. Jane Smith, an infectious disease specialist, states, “The identification of a sexually transmitted fungal infection is a wake-up call for both the public and healthcare providers. We must prioritize education on safe sexual practices and promote regular health screenings to detect and treat infections early.”
Healthcare professionals are closely monitoring the situation to assess the likelihood of further cases. While this first case is concerning, it also provides an opportunity to enhance surveillance and research efforts. Dr. John Doe, an epidemiologist, notes, “Continued vigilance and research are essential to understand the transmission dynamics of this infection and develop effective prevention strategies.”
Implications for Public Health and Future Research
The emergence of the first sexually transmitted fungal infection in the U.S., identified in New York City, presents significant public health challenges. Effective management and containment of this infection require a multifaceted approach, addressing both immediate and long-term concerns. Public health officials must prioritize rapid identification and isolation of cases to prevent widespread transmission. Comprehensive sexual health education is essential, emphasizing the potential risks and encouraging safe practices.
One of the immediate challenges is the lack of awareness and diagnostic tools specific to this fungal infection. Healthcare providers need targeted training to recognize symptoms and employ the appropriate diagnostic techniques. Strengthening laboratory capacities for fungal testing and reporting is critical. Moreover, public health campaigns should be launched to inform the public about this new threat, promoting early reporting of symptoms and seeking medical advice.
Future research must focus on multiple aspects of this infection. Understanding its origins is paramount to prevent further cases. Investigating the genetic and environmental factors contributing to its transmission can provide insights into its spread and help develop targeted interventions. Research should also aim to identify effective treatments, as current antifungal therapies may not be fully effective against this novel pathogen.
Prevention strategies are equally important. Developing vaccines or prophylactic treatments could offer long-term solutions to control the infection. Additionally, public health policies should be updated to include fungal infections in sexually transmitted infection (STI) screening programs. Collaborative efforts between government agencies, healthcare providers, and researchers are crucial to build a robust response framework.
The discovery of this fungal infection underscores the importance of vigilance and readiness in addressing emerging health threats. Continuous surveillance, prompt reporting, and a proactive stance in research and public health initiatives will be key to mitigating the impact of this and future infectious diseases.
OUR SITE: toinewsalert.com